This article explores the role of waste management in the drive for a net-zero NHS
The NHS is responsible for 6.3% of England’s total carbon emissions – producing the same amount of CO2 every year as over 80,000 space shuttle launches. And, while only accounting for around 0.1% of these emissions, waste is a major issue that will need to be addressed if the health service is to meet the Government’s net-zero ambitions. The COVID-19 pandemic, in particular, has added to waste streams as single-use PPE and medical devices are favoured over reusable products. To help trusts improve waste management, the Royal College of Physicians recently published Less waste, more health: A healthcare professional’s guide to reducing waste, which emphasies the importance of reducing, reusing, and recycling. It states: “In England, there are 165 hospital trusts with a combined expenditure of over £4.6bn per annum on medical supplies and other consumables. “Improving environmental practices in manufacturing and distribution will minimise impacts on environmental factors such as air quality, ultimately improving health. “Redirecting, or minimising waste, can also secure financial savings that can be reinvested into patient care.” Backed by NHS Improvement, it will support NHS organisations in delivering £150m annual efficiency savings, with a substantial contribution coming from identifying better waste management practises.
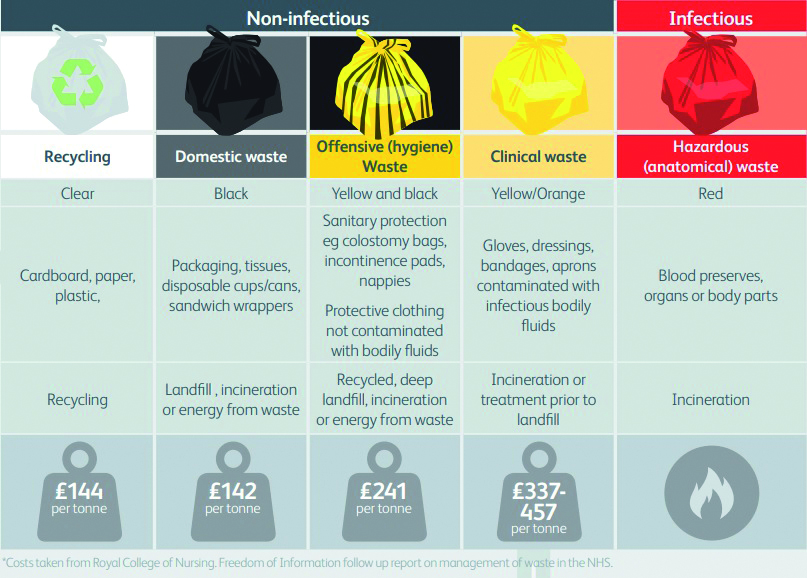
Correct classification
The first step in this effort is ensuring correct classification so that less waste needs to be incinerated. Kim Ormsby, assistant director at waste management specialist, Anenta, explains: “Ensuring that all healthcare waste is segregated correctly, including the use of the offensive waste ‘tiger bags’, is a vital step. This will reduce the amount of waste that is sent for incineration and will increase the amount that is sent to alternative technology and energy- from-waste providers.” Graeme Knight, director at B&M Waste Services, adds: “With a critical lack of high-temperature incineration in the UK, disposal costs of hazardous wastes are increasing, therefore it is more important than ever to accurately classify your waste and reduce the amount sent as ‘hazardous’ or ‘offensive’ through correct segregation. “The result can be financially rewarding for those in the health sector at a time when we know NHS budgets are particularly tight. “Not only this, our customers often also see increases in recycling levels, as trained staff place items in recycling bins as opposed to clinical waste containers. This will then be 100% recycled, or have energy recovered from it, as opposed to being incinerated or sent for deep burial, and at a much-cheaper rate than clinical waste disposal.”
Embracing innovation
The knock-on effect of better management will be a reduction in CO2, according to Alice Woodwark, managing director of communities at Mitie. She told hdm: “As with any sector, the best way to improve waste management and reduce the associated carbon emissions is to prevent as much potential waste entering a site as possible. “However, this is increasingly complex in clinical environments, so hospital waste management is a critical part of the overall healthcare management. “Any materials that have to be created, especially anything intended for single use, has a carbon impact associated with its production and disposal, so it’s vital that hospitals and other healthcare environments find innovative ways to reduce their carbon footprint by developing and implementing strategies, technologies, and processes that reduce this impact and help drive the sector’s quest to achieve zero waste and net-zero carbon emissions.”
Making an impact
Quick wins, she said, include implementing electronic meal ordering software on wards to ensure only the exact number of meals needed are prepared. And, while it may be more challenging to reduce some aspects of waste in clinical environments, focusing on waste in back-office areas will also make a significant impact. “Simple things, such as ensuring there’s appropriate provision for recycling and food waste, up to ensuring resources such as furniture is recycled or donated elsewhere for a second life rather than going to landfill, all have a positive impact,” said Woodwark.
The war on plastics
Mitie has worked with a number of trusts to help improve waste management. These include St George’s University HospitalsNHS Trust Foundation, which has implemented a low-carbon menu for patients aimed at reducing waste and the associated carbon emissions. It is estimated to have saved up to 23 tonnes of CO2 a year. And The Dudley Group NHS Trust Foundation has removed all single-use plastic items from its catering service. By switching to alternative products, Mitie and the trust cut the number of single-use plastic items being used at the hospital from approximately 1.8 million a year to 300,000.
Education, education, education
As well as better segregation of waste, educating staff, patients, and visitors will be key. James Cardwell-Moore, senior director at Stericycle, said: “Every day, frontline health workers decide how items are either reused, recycled, or treated as general or healthcare waste. “Ensuring correct placement of containers, appropriate segregation, and the safe and sustainable handling of clinical waste will help protect staff and patients while contributing to net-zero targets by minimising the impact on our environment, including climate change.” Ormsby added: “The biggest source of poor waste management is a lack of awareness. “Staff with low waste stream awareness will have a tendency to dispose of waste incorrectly, or simply in the bin closest to them. “Conversely, well-deployed waste training will result in high levels of awareness that will streamline waste segregation properly, maximising waste that can be recycled. “Staff engagement, including the buy-in of those at a senior level, is critically important. Without a team that buys into proper segregation of waste, cultural change cannot be affected.”
Taking responsibility
To encourage and educate staff, in particular, Initial Medical advises placing segregation posters at all disposal points and investing in more recycling bins. And Ormsby said trusts should ensure that a board member has responsibility for waste; that there is a dedicated waste manager; and that a robust waste management policy is in place and available to all. “Providing training as part of core staff training is key, and regular audits will help to avoid any bumps in the road and keep you on track to achieving net-zero goals,” she said. “Waste is an unavoidable facet of healthcare and needs to be given the appropriate resource to ensure that it is being segregated and disposed of correctly. This will reduce the amount of mis-segregation and enhance the amount of energy generated from correctly-segregated waste.” Waste audits are also becoming increasingly popular. These are undertaken at least once a year to identify issues that need addressing.
A duty of care
To support trusts Anenta has developed a bespoke waste audit app, designed to reduce the need for onsite reviews by external bodies. “The app enables producers of healthcare waste to meet their statutory obligations, taking users through a step-by-step process, including how to conduct compulsory clinical waste pre- acceptance audits, and duty of care audits,” explains Ormsby. “This streamlines the waste audit process, saving time and dramatically cutting costs, saving between £300- £800 on physical audits and condensing the audit process to just 40 minutes as opposed to up to six days.” Woodwark adds: “When it comes to reducing carbon emissions, no activity is too small or insignificant, and quick wins are often the key catalysts in kickstarting greater net-zero carbon efforts.”