
This article explores how data collection and technology are helping hospitals to maximise their response times to patient alarms, improving staff efficiency and patient outcomes
Hospital design has evolved in recent years, with largely single- room inpatient facilities replacing multi-bed bays. And this approach became critically important at the height of the Coronavirus outbreak, when hospitals were forced to segregate patients to prevent the further spread of infection. But, while offering patients greater privacy and dignity, and a quieter and more-personal environment in which to recover; it also has its challenges – primarily around monitoring and communication. Visitors to any hospital will be all too familiar with the plethora of alarms sounding to alert staff to patient requests and the potential failure of life- saving medical machinery. Especially in hospitals with a greater proportion of single-room patient accommodation, responding to these alarms can prove difficult and led to 3,266 claims against the NHS for inadequate care between 2016-2021, costing trusts a staggering £247m, according to figures released by NHS Resolution. And the situation is not improving.
The scale of the problem Last year the Health and Safety Investigation Branch (HSIB) examined the case of a 73-year-old man who was admitted to hospital in December 2020 with COVID-19. He died alone in a hospital side room after his breathing equipment became disconnected and his calls for help via his bedside nurse call system went unheard. In its report, the HSIB said the ward was ‘extremely busy’ at the time because of staff shortages, a new patient arriving on the ward, and ‘competing clinical priorities’. And its investigation stated that ‘caring for such acutely-unwell patients in side rooms on general wards poses a safety risk’. Technology giant, Philips, also has a case study on its website telling the story of premature baby, James, who spent six months in a neonatal intensive care unit. His mother recalls: “It seemed that whenever his nurse turned away from his incubator to care for another baby, she couldn’t get more than a couple of meters away before James’s alarm sounded, insisting that she turn around again.” Often these alerts were false alarms, but when James was four months old, and during a staff shift change, the alarm went off, signalling that his condition was deteriorating. “We pushed the emergency call button, but nobody answered it,” his mother recalls. “As our son started to turn blue before our eyes, my husband and I tore through the NICU to find someone to flag down. “Not seeing anyone, I ran out to the receptionist so she could call for help. “A nurse appeared and called for a crash cart. When the crash cart came, it came agonisingly slowly, and by then James was grey-blue and motionless. It took several more excruciating minutes to revive him.” Inevitably, that single event changed the dynamic between the family and James’s care team, and a great amount of trust was lost. His mother said: “I think alarm fatigue can still negatively impact family members’ relationships with the healthcare team and cause them to lose faith in the hospital as a whole.
Life-threatening delays “Nurses know better than anyone that 99 out of 100 alarms may not require immediate attention. But what they might not know is how parents can interpret delayed reactions to alarms as complacency and unreliable alarms as indicative of untrustworthy equipment. “Sometimes I felt that nurses silenced alarms as a reflex, and I noticed that every nurse had vastly different reaction times and levels of concern when it came to his alarming. “Some nurses set his parameters differently, being personally comfortable with a wider margin; and a few even gave us permission to push the silence button ourselves if we determined it to be a bad read. “While it was nice to be able to quiet the squalling alarms on our own without waiting for a nurse, having that responsibility didn’t instil confidence that there were consistent policies in place to keep James safe.” While these are two extreme examples of the consequences of alarm fatigue, they highlight an issue which hospitals need to deal with. With this problem in mind, the Association for the Advancement of Medical Instrumentation has published the Clinical Alarm Management Compendium to provide evidence- based advice on safer alarm management. It calls for greater leadership and management, improved data collection, and increased effort to train and educate staff.
Greater leadership And, increasingly, hospitals are turning to modern technology to address the problem. Chesterfield-based Tutum Medical has developed the multi-award-winning Bedside Equipment Alarm Monitoring System (BEAMS), an innovative new solution specifically designed for single-bed patient rooms and four- to six-bay hospital wards. Having been installed in single rooms across wards at Sheffield Children’s Hospital, and now being trialled in a number of other hospitals across the UK, BEAMS integrates a digital platform with audible monitors, a speaker system, and nurse consoles. It is also mains-operated and creates its own Wi-Fi mesh network, which removes the need to interface to hospital infrastructure. And in trials it has been found to significantly improve response times for bedside critical alarms, leading to improved patient outcomes, better workflow for nurses, and reduced healthcare costs for the hospital. Importantly, BEAMS can also identify ambient and irrelevant background sounds in a patient’s room, alerting nurses only when a recognisable medical alarm is triggered indicating patient distress. And the unit is suitable to install within any hospital room and will not disturb patients or staff with unnecessary sounds and alerts.
Tailored solutions In addition, it has a default delay of 40 seconds prior to alerting the duty nurse to minimise alarm fatigue, and this can be tailored to suit specific healthcare practices and environments. Results from the trial at Sheffield Children’s Hospital showed a reduction in the average time taken for a patient requiring care to be seen by a nurse of 6.43 minutes when alerted by BEAMS. The maximum time taken for a patient to be seen by a nurse prior to installing the BEAM system was 90 minutes. But, through the use of the BEAMS unit, this time was reduced by 75 minutes – with the maximum duration a patient waited for nurse attention dropping to 14.15 minutes. Rawlinson said: “This clinical trial demonstrated that BEAMS produced an 84% reduction in the maximum response time to alarms and a 74% reduction in average alarm response times overall. “It is the combination of superior hardware and state-of-the-art technology that allows BEAMS to reduce staff response times, improve patient care, and increase staff productivity.”
Intercall has also created a platform to address the issue of alarm fatigue.
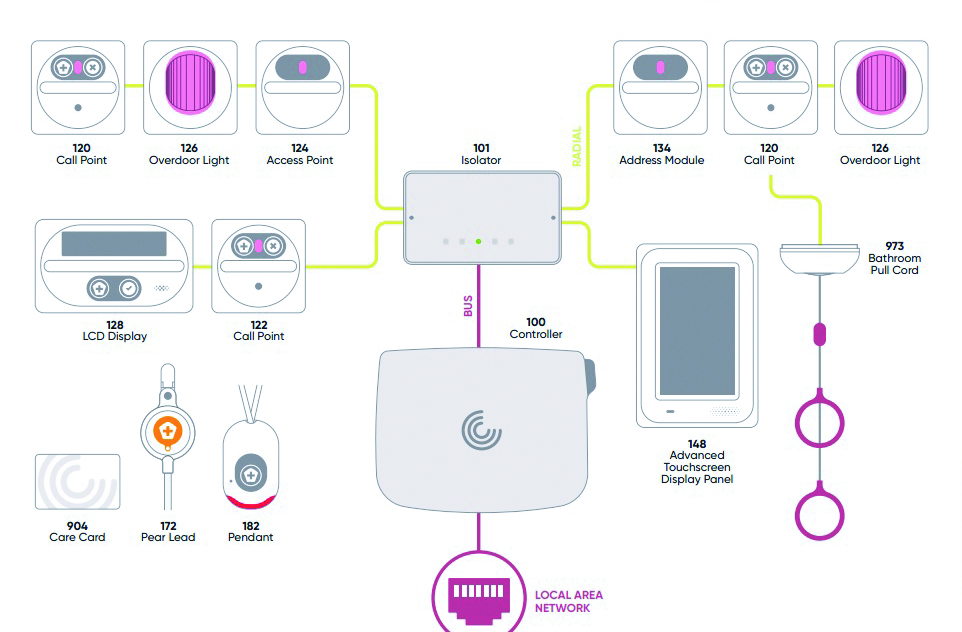
Intercall One features call points, touchscreen displays, pull cords, wearable pendants, passive infrared detectors, isolators, call points, and overdoor lights with sounders to deliver real-time accurate call data to the right people, in the right place, at the right time, ensuring a prompt response.
And the system is supported with Intercall Care cards to identify staff and record actions.
Philips is also supporting hospitals with a Clinical Services team that uses clinical analytics, environmental and process assessments, and technology to drive workflow optimisation and organisational improvements.
Data collection A spokesman said: “Non-actionable alarm signals are often caused by motion artifacts, manipulation of the patient or patient movement, inappropriate alarm limits, or faulty technology and can divert time and attention away from patients.
“Our solution can be configured to alert caregivers when vital signs reach chosen thresholds and to remain silent when events are non-actionable.”
When Philips IntelliVue patient monitoring system was installed in the ICU department at St Antonius Hospital in The Netherlands, non-actionable alarms were reduced by 40%.
The spokesman said: “In the former ICU facility, the team was very aware of the many negative consequences of alarm fatigue for patients and staff.
“They had taken steps to reduce their irrelevant alarms, and experienced fewer of them, but had never measured their improvement.
A whole-system approach “When they moved to a new ICU facility, they equipped it with new Philips IntelliVue monitoring systems.
“A configuration setting was carefully chosen, which led to a further reduction of alarms, but the department felt they could do more and they asked the Clinical Services team to see if they could find ways to further reduce their irrelevant alarms.
“Different stakeholders were interviewed and Philips consultants then measured the specific number of alarms generated in the ICU ward over the period of a week to establish a baseline for the project.”
This work revealed 344 alarms per bed patient per day. And, more worrying, was the number that were ignored, silenced, or turned off.
The ICU now offers improved training for all staff and has introduced a second alarm profile for medium-care patients which is helping to further reduce unnecessary alarms.
Ineke van de Pol, project champion and ICU nurse practitioner, said: “When an alarm goes off you want to make sure it is clinically relevant.
“Our entire focus was on separating the clinically-relevant alarms from non-clinically relevant alarms.”
These improvements allowed the ICU team to reduce the number of alarms by 27%, from 344 to 249 alarms per bed, per day.
Arrhythmia alarms were reduced by 47% and SP02 alarms by 54%.
Van de Pol said: “We all thought that the alarms weren’t such a big issue, but we didn’t realise just how big the problem was, or how much better we could make the situation.
“The Philips Clinical Consultants really helped us with that.
“You absolutely have to have the data to know what your actual situation is and to improve it. That also motivates everyone to make changes.”
